BACKGROUND: We previously reported early efficacy and 5-year follow-up of a multicenter phase 2 study of lenalidomide plus rituximab as initial treatment for MCL (NEJM 2015:373:1835; Blood 2018:132:2016), which was highly effective (ORR 92%, CR 64%) and well tolerated, with durable responses (5-year PFS and OS of 64% and 77% respectively). Here we present 7-year follow up analysis.
METHODS: This study included both induction and maintenance with lenalidomide (L) and rituximab (R). During induction, patients received lenalidomide 20 mg daily on days 1-21 of a 28-day cycle for 12 cycles, followed by maintenance with dose reduction to 15 mg. Patients received rituximab weekly for four weeks during cycle 1, then once every other cycle. Treatment continued until progression of disease, with an option to stop therapy after 3 years.
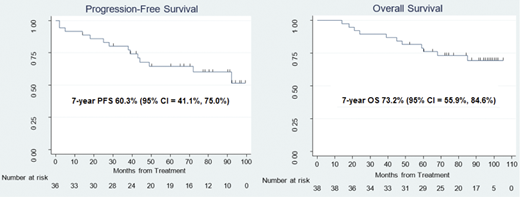
RESULTS: A total of 38 subjects requiring therapy were enrolled at 4 centers from 7/2011 to 4/2014. Median age was 65 with MIPI scores evenly distributed between low-, intermediate-, and high-risk groups. As of July 2020, the median follow-up was 86 months with range of 73-105 months. Two patients were inevaluable - one withdrew consent and the other was intolerant of tumor flare during induction. Nineteen (53%) of the evaluable 36 patients remain in remission, including 12 (33%) beyond 7 years. Of the patients in remission, 12 (33%) remain on treatment, including 4 on both L+R (at 100, 97, 96, and 92 months of treatment), 7 on R alone (105, 101, 98, 97, 92, 84, and 77 months), and 1 on L alone (72 months), while 7 patients in remission opted to stop therapy after at least 3 years of study treatment due to side effects or patient preference. Fourteen patients had progression: 3 had primary refractory disease and 11 relapsed following initial responses (5 CRs with PFS of 18, 38, 39, 49, and 72 months, 6 PRs with PFS at 14, 25, 28, 43, 44 and 92 months). Eleven evaluable patients have died, 8 from lymphoma progression and 3 from unrelated comorbidities. Eleven total patients stopped therapy while in remission: 7 remain in ongoing remission while off treatment for 0, 11, 15, 17, 29, 51, and 55 months, 1 progressed after 19 months off of therapy, and 3 died of causes unrelated to lymphoma. Median PFS and DOR have not been reached. The 7-year PFS rate was estimated at 60.3% (95% CI = 41.1%, 75.0%) with 7-year OS rates at 73.2% (95% CI = 55.9%, 84.6%). Interestingly, MIPI score ≤6.2 was predictive of increased overall survival (p = 0.04), with 7-year OS rates of 80.6% in this group versus 57.1% in patients with MIPI >6.2, while there was no difference in PFS between the two groups. Ki67 <30% at diagnosis was not predictive of PFS or OS. TEAEs during maintenance included asymptomatic grade 3-4 cytopenias (42% neutropenia, 5% thrombocytopenia, 3% anemia), and grade 1-2 infections (50% URI, 21% UTI, 16% sinusitis and 16% cellulitis), all managed in outpatient settings. Two patients (5%) developed hypogammaglobulinemia requiring discontinuation of rituximab. Seven patients required brief hospitalization for IV antibiotics: 1 (3%) developed neutropenic fever in setting of cholecystitis, 5 (13%) had pneumonia and 1 (3%) had recurrent UTI. Secondary primary malignancies (SPM) were mostly cutaneous. One Merkel-cell carcinoma developed in an 86-year-old subject after 18 months of therapy, and one pancreatic cancer was diagnosed in a 68-year-old patient after 12 months of therapy. No invasive SPM was reported beyond 2 years on treatment.
CONCLUSIONS: Lenalidomide and rituximab as initial treatment for MCL can achieve high rates of complete responses with durable remissions in both elderly and younger patients, with many patients maintain remissions now extending beyond 7 years. Toxicity was not significantly affected by continuous treatment, and close follow up was able to limit toxicity for those who wished to remain on therapy. It is notable that this combination offers a chemotherapy-free initial approach which compares favorably in outcome to conventional outpatient chemotherapy-based regimens such as bendamustine-rituximab, VR-CAP, and R-CHOP with rituximab maintenance. Further evaluation of this active regimen in larger, randomized frontline trials comparing novel agents with chemoimmunotherapy is warranted. (ClinicalTrials.gov - NCT01472562)
Martin:Janssen: Consultancy; Bayer: Consultancy; Beigene: Consultancy; Cellectar: Consultancy; Morphosys: Consultancy; Regeneron: Consultancy; Karyopharm: Consultancy, Research Funding; Sandoz: Consultancy; I-MAB: Consultancy; Kite: Consultancy; Incyte: Consultancy; Teneobio: Consultancy; Celgene: Consultancy. Shah:NCCN: Vice-Chair, Acute Lymphoblastic Leukemia Working Group: Membership on an entity's Board of Directors or advisory committees; Kite/Gilead, Precision Biosciences, Novartis, AstraZeneca: Other: TRAVEL, ACCOMMODATIONS, EXPENSES; Kite/Gilead, Celgene/Juno/BMS, Novartis, Pfizer, Amgen, Spectrum/Acrotech, Precision Biosciences, Beigene, AstraZeneca, Pharmacyclics/Jansen, Adaptive: Honoraria; Moffitt Cancer Center: Current Employment; Kite/Gilead, Jazz, Incyte: Research Funding. Schuster:AlloGene, AstraZeneca, BeiGene, Genentech, Inc./ F. Hoffmann-La Roche, Juno/Celgene, Loxo Oncology, Nordic Nanovector, Novartis, Tessa Therapeutics: Consultancy, Honoraria; Novartis, Genentech, Inc./ F. Hoffmann-La Roche: Research Funding. Smith:Acerta: Research Funding; Celgene: Consultancy, Research Funding; BMS: Consultancy; Pharmacyclics: Research Funding; Genentech/Roche: Consultancy, Other: Support of parent study and funding of editorial support, Research Funding; Janssen: Consultancy; FortySeven: Research Funding; TG Therapeutics: Consultancy, Research Funding; Karyopharm: Consultancy, Research Funding. Svoboda:Astra-Zeneca: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Imbrium: Consultancy; Incyte: Research Funding; Merck: Research Funding; Pharmacyclics: Consultancy, Research Funding; Seattle Genetics: Consultancy, Research Funding; TG: Research Funding; Genmab: Consultancy; Adaptive: Consultancy; Atara: Consultancy. Furman:AstraZeneca: Consultancy, Research Funding; Beigene: Consultancy; Genentech: Consultancy; Sunesis: Consultancy; TG Therapeutics: Consultancy, Research Funding; Verastem: Consultancy; Incyte: Consultancy; Pharmacyclics: Consultancy; Oncotarget: Consultancy; Loxo Oncology: Consultancy; Janssen: Consultancy, Speakers Bureau; Acerta: Consultancy; Abbvie: Consultancy. Rutherford:Seattle Genetics: Consultancy; Genentech/Roche: Research Funding; Dova: Consultancy; Heron: Consultancy; Karyopharm: Consultancy, Research Funding; Juno: Consultancy; AstraZeneca: Consultancy; Celgene: Consultancy; LAM Therapeutics: Research Funding; Kite: Consultancy; Regeneron: Research Funding. Allan:Acerta, Genentech, Abbvie, Sunesis, Ascentage, Pharmacyclics, Janssen, AstraZeneca, BeiGene: Consultancy; Abbvie, Janssen, AstraZeneca, Pharmacyclics: Honoraria; Celgene, Genentech, Janssen, TG Therapeutics: Research Funding. Leonard:Sutro: Consultancy; Gilead/Kite: Consultancy; Roche/Genentech: Consultancy; BMS/Celgene: Consultancy; Regeneron: Consultancy; ADC Therapeutics: Consultancy; Bayer: Consultancy; MEI Pharma: Consultancy; GenMab: Consultancy; Karyopharm: Consultancy; AstraZeneca: Consultancy; Epizyme: Consultancy; Miltenyi: Consultancy. Ruan:AstraZeneca: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Pharmacyclics: Research Funding; Kite Pharma: Consultancy; Seattle Genetics: Research Funding; Juno: Consultancy; BMS: Consultancy, Research Funding.
This presentation will discuss the use of lenalidomide in untreated mantle cell lymphoma
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal